Pharmacotherapy
Contents
Pharmacotherapy
Modify the biological processes that underpin the motivation to take drugs.
e.g. some block the neural substrates of reward - i.e block the euphoric effects
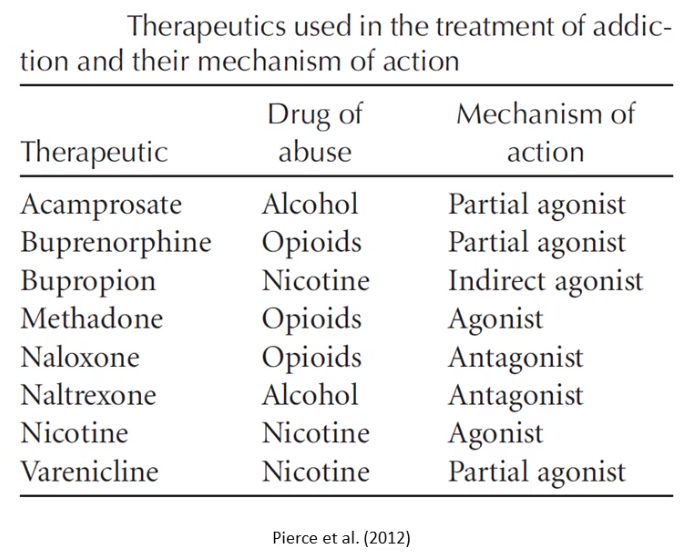
Agonist - activate receptors to increase their function (by excitation or inhibition)
Antagonist - block the action of the neurotransmitter.
Full agonist - activates a receptor to its maximum
Partial agonist - function as a 'competitive antagonist' by occupying receptors
Indirect agonist - enhance the function of neurotransmitters without activating the receptors for the transmitter (i.e. blocking transports, inducing release inhibiting metabolism)
Alcohol increases NT GABA, decreases the NT glutamate -> reduce activity across the nervous system. Chronic occupancy can result in downregulation or desensitisation where withdrawal from alcohol will result in a lack - dangerous!
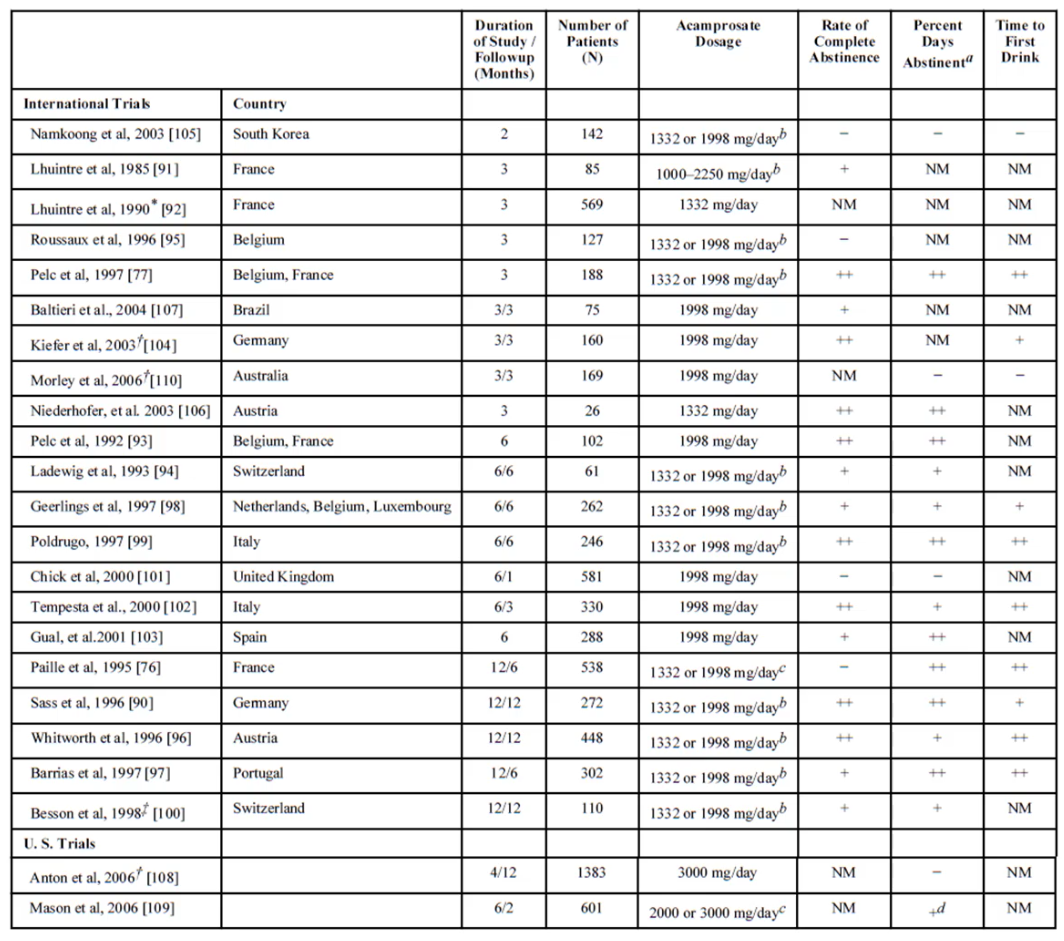
Acamprosate - A GABA agonist and glutamate NMDA antagonist - that can oppose the neural effects that may have happened following alcohol withdrawal
Boismare et al (1984) gave rats acamprosate, and found that they reduced alcohol consumption
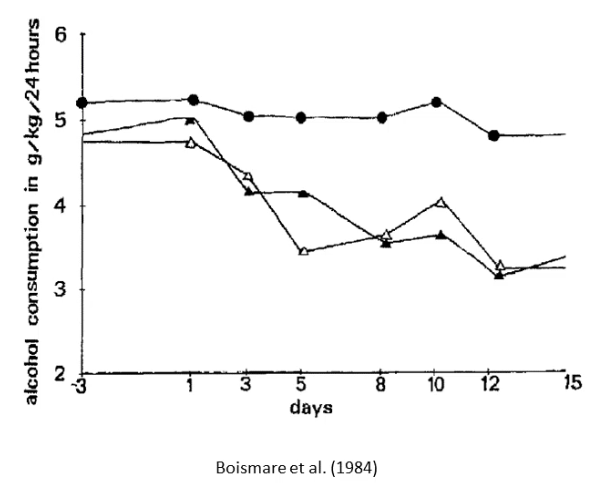
- Filled circles - placebo control group
- Triangles - different dosages
Unclear of the whether acamprosate reversed withdrawal or competed with direct rewarding effects of alcohol.
Mason and Heyser (2010)
Showed that there is a significant effect of the use of acamprosate
Increased abstinence rates by about 10-20% over 80 days following the quit date
Naltrexone
An antagonist of opioid receptors, blocking the function of endogenous endorphins.
First studied for alcohol dependence in the 1970s, following discovery of the role of opiate receptors in opiate dependence.
Naltrexone + Acamprosate = Additive treatment effects, broader protection from relapse
Maisel et al 2013 found that acamprosate increased the number of abstitenent days more than naltrexone, but naltrexone reduced craving and heavy drinking sessions.
Acamprosate makes the effects of withdrawal less bad
Naltrexone blocks the euphoric effects of alcohol, reducing craving and heavy use
Disulfiram (Antabuse)
Treatment for alcoholism
Blocks acetaldehyde dehydrogenase (a liver enzyme that breaks down alcohol), increases the sensitivity to alcohol consumption - causing them to consume less of the alcohol to feel the same effect.
Dangerous for those who take it unknowingly
Hard to make clients comply and continually take it.
- Attempted depot treatment (slow down the release so that it can be taken less frequently)
Now rarely used as treatment (Heilig & Egli 2006)
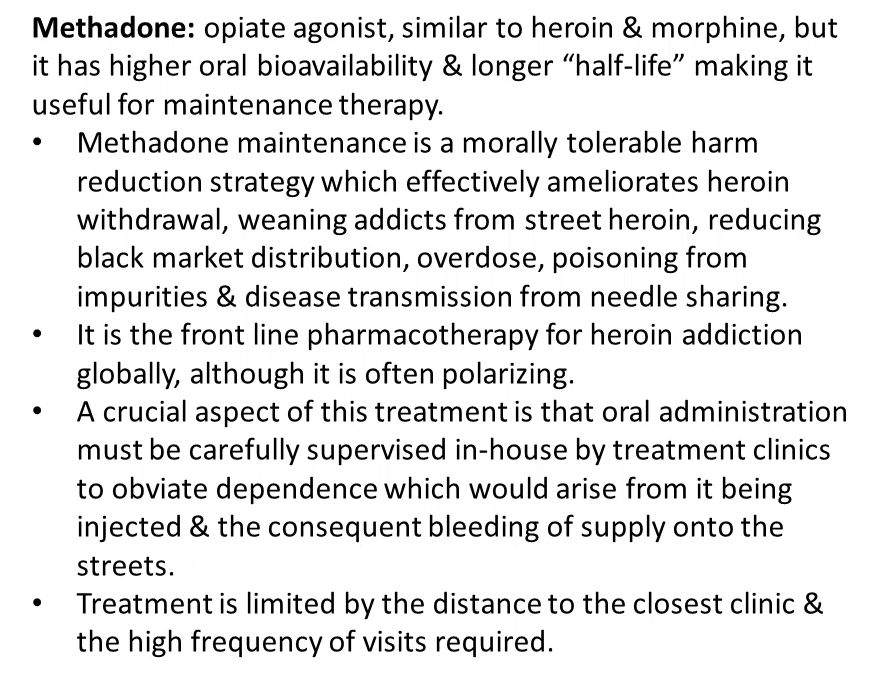
Methadone
For treating heroin and opiate dependence.
Has a higher oral bioavailability and longer half-life, making it useful for maintenance therapy.
Needs to be closely monitored by professionals - need regular visits to a clinic
Suboxone
Developed so that opiate addicts do not need to regularly visit a clinic.
Combination of buprenorphine (partial opiod receptor agonist with a good oral bioavailability) and naloxone (opiod receptor antagonist).
As naloxone has a poor oral bioavailability, the administration of suboxone is more rewarding as a result of the buprenorphine.
If injected, the naloxone counters the opioid agonist effects, making the injection unrewarding.
This causes suboxone to be taken orally more pleasurably than via injections.
Nicotine Replacements
In 1967, Dr Claes Lundgren suggested nicotine as a substitute for tobacco, having seen sailors switch from smoking to chewing tobacco
Ove Ferno designed nicotine gum as a means to orally administer nicotine with delayed absorption.
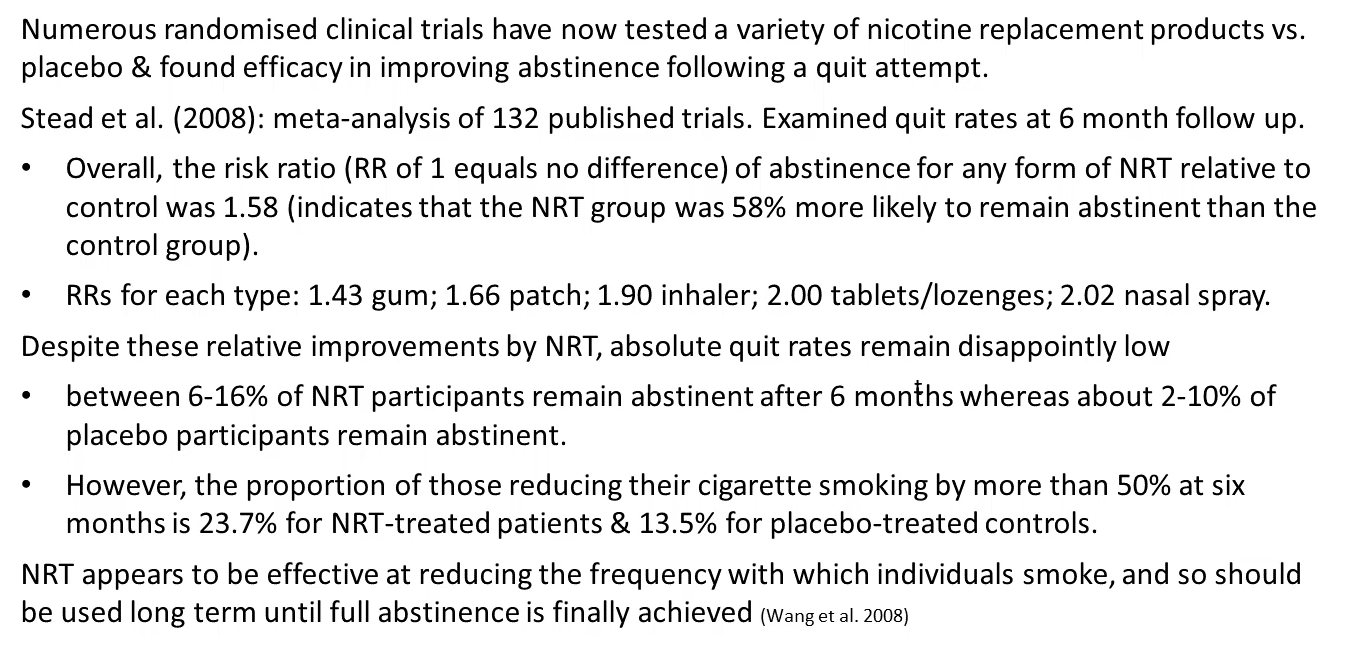
Abstinence increased a lot, however it did not improve absolute quit rates.
However, effective at reducing the frequency of smoking (Wang et al 2008)
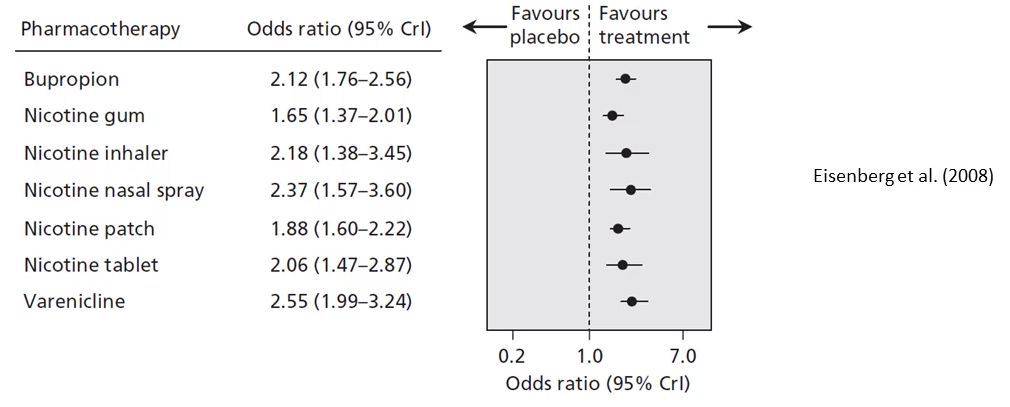
Bupropion (Zyban)
Bupropion is a dopamine, noradrenaline indirect agonist // reuptake inhibitor, and antagonist for nicotine acetylcholine receptors. Blocks the rewarding effects of nicotine, rather than by reversing withdrawal induced depression - which may improve abstinence rates
Tobacco withdrawal syndrome is associated with a marked increase in depression, which furthers the inability to quit smoking
Anti-depressent agents may protect against relapse by decreasing depression tendency.
Hurt et al (1997) found that the anti-depresant bupropion produced superior quit rates, marketed as a smoking cessation agent under the name Zyban.
Varenicline (Champix)
Acetylcholine partial agonist - weak nicotine replacement agent to make acetylcholine neurons reverse withdrawal related hypofunction, and blocks the rewarding effects of smoking by competing with nicotine.
Demonstrated to be slightly more effective as a smoking cessation agent than NRT or bupriopion. Though absolute quit rates still remain low
Gabapentin
THC activates CB1 receptors to inhibit other cells, increasing over brain inhibition. Following cannabis withdrawal, the brain over-excitates.
Gabapentin seems to help to reduce both cannabis use and withdrawal
Treatments
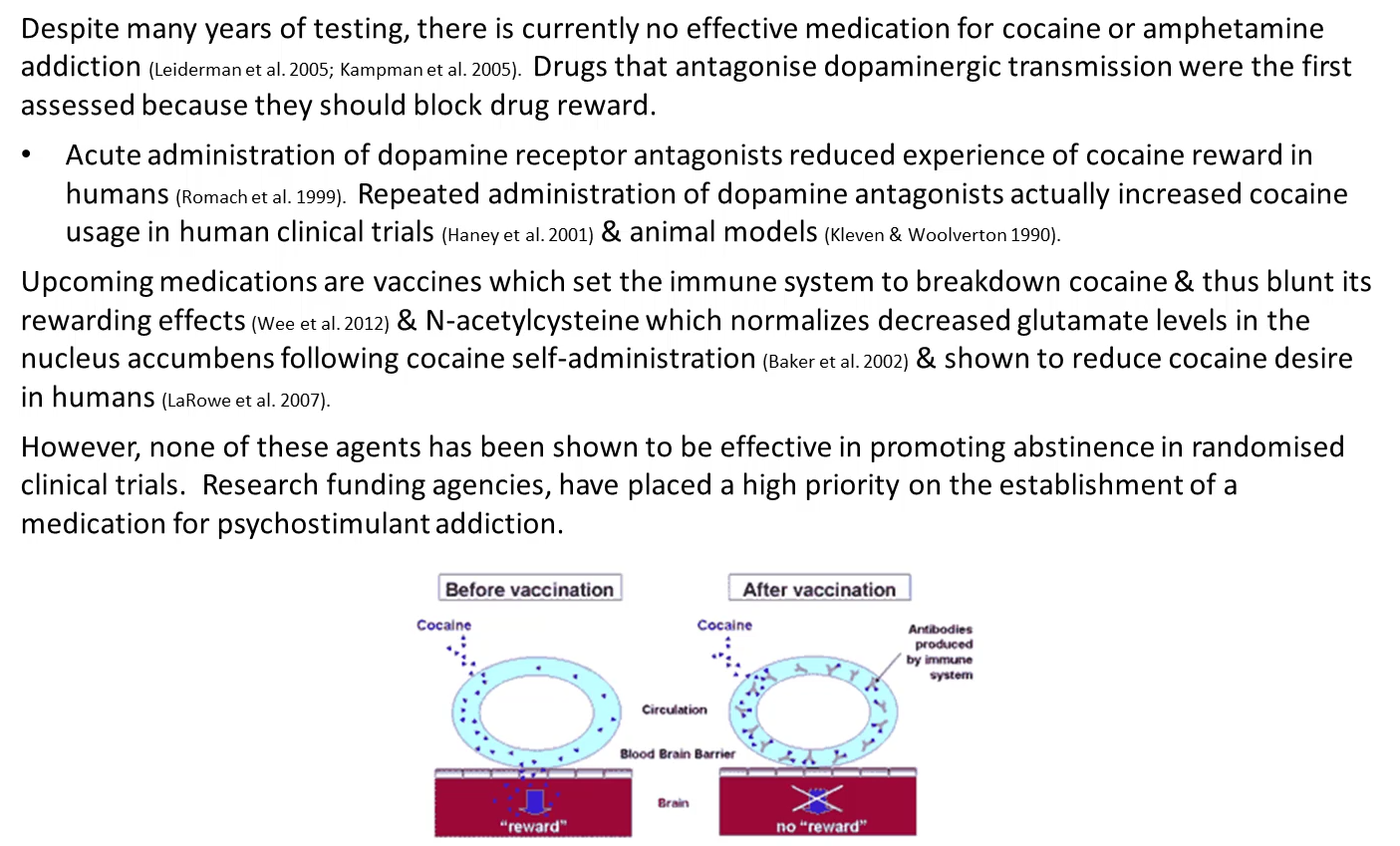
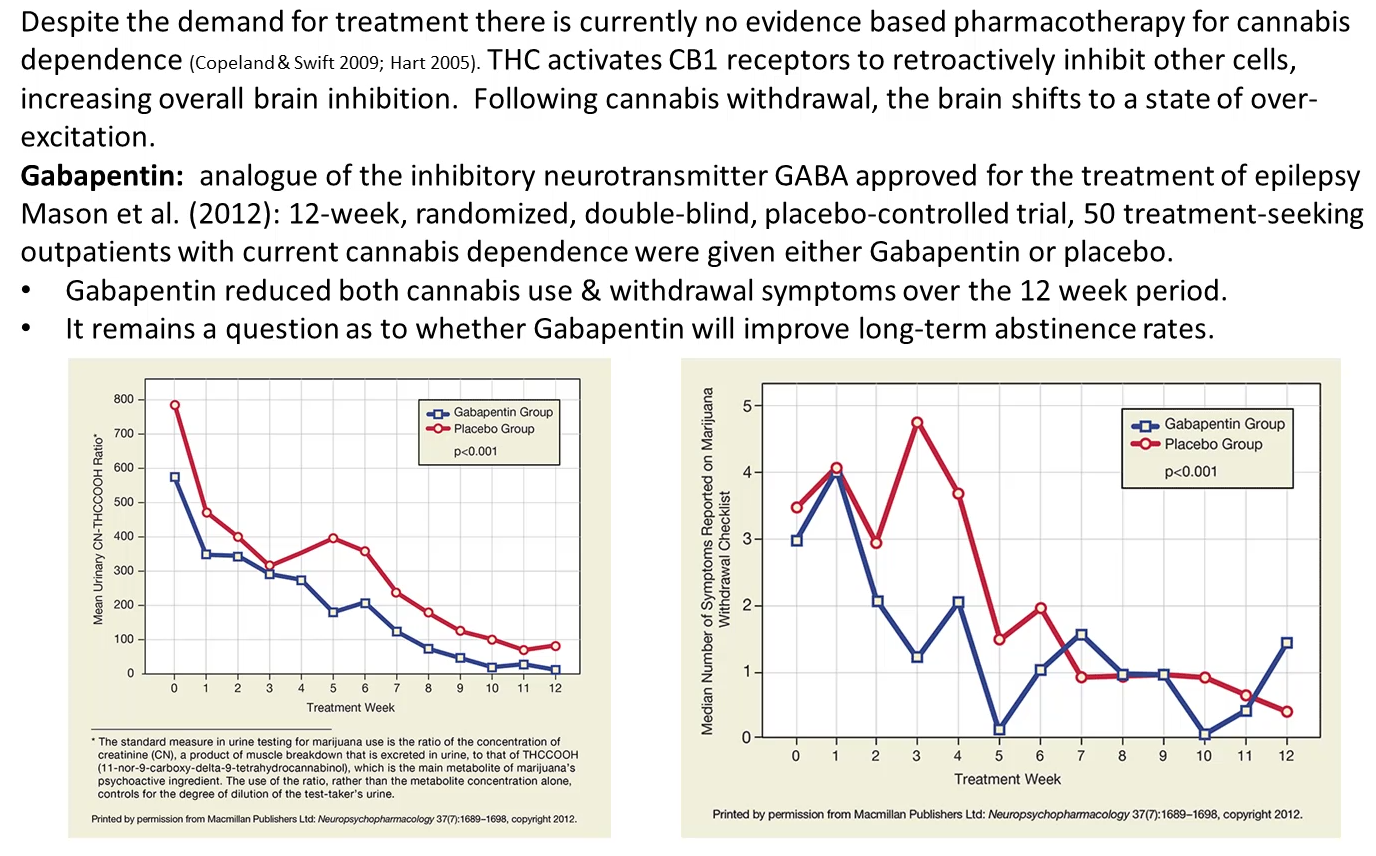
Currently no effective medication against cocaine, amphetamine or cannabis addiction.
Cognitive Enhancers
Drugs that improve performance on some metric
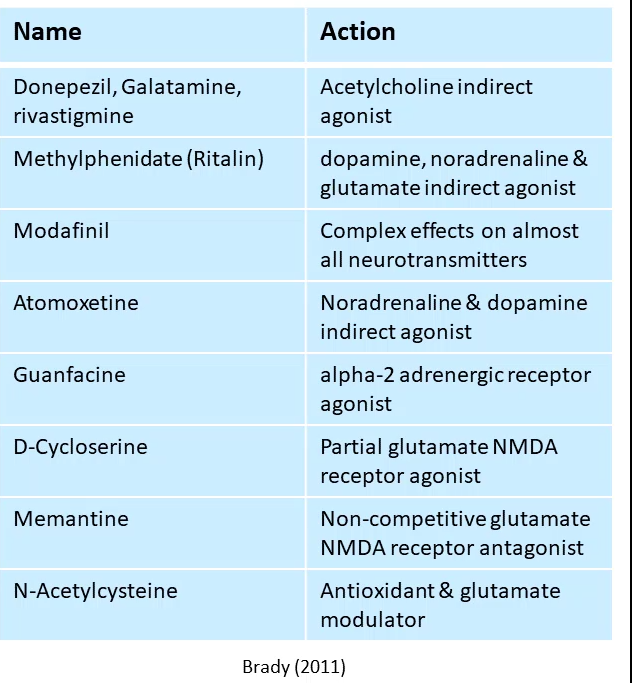
None of them have compelling efficacy to treat addiction